
July 2024
Introduction and background
In a space as competitive as the Group Benefits market, where carriers strive to offer the best product, price, capabilities, and service, innovation is often necessary to deliver strategic advantage. This is especially true when brokers expect rapid quotes and often provide limited data to enable underwriters to assess risk accurately. What if some of the uncertainty could be taken out of underwriting and pricing through technology-enabled risk evaluation? What if we could leverage medical data to offer competitive yet profitable rates for cases through mortality risk segmentation? Let’s find out how.
Data has always been integral to the group underwriting process. However, as new data sources emerge, traditional sources alone are no longer enough. Carriers are aware of the need to expedite the expansion of their digital capabilities to generate continuing growth. A data-driven approach using predictive models for rapid and accurate risk evaluation, leveraging third-party data to enhance traditional census data, is the future of group underwriting.
The following case study evaluates one data-enhanced approach to Group Life underwriting. This method utilizes third-party medical data enrichment of traditional census data for a Group Life carrier, followed by mortality risk assessment through a predictive model. The aim is to assist underwriters to:
- Efficiently prioritize business to focus on the right cases and broker relationships
- Confidently provide competitive rates for cases in target markets
The results are a proof of concept to supplement current underwriting methods.
Study methodology
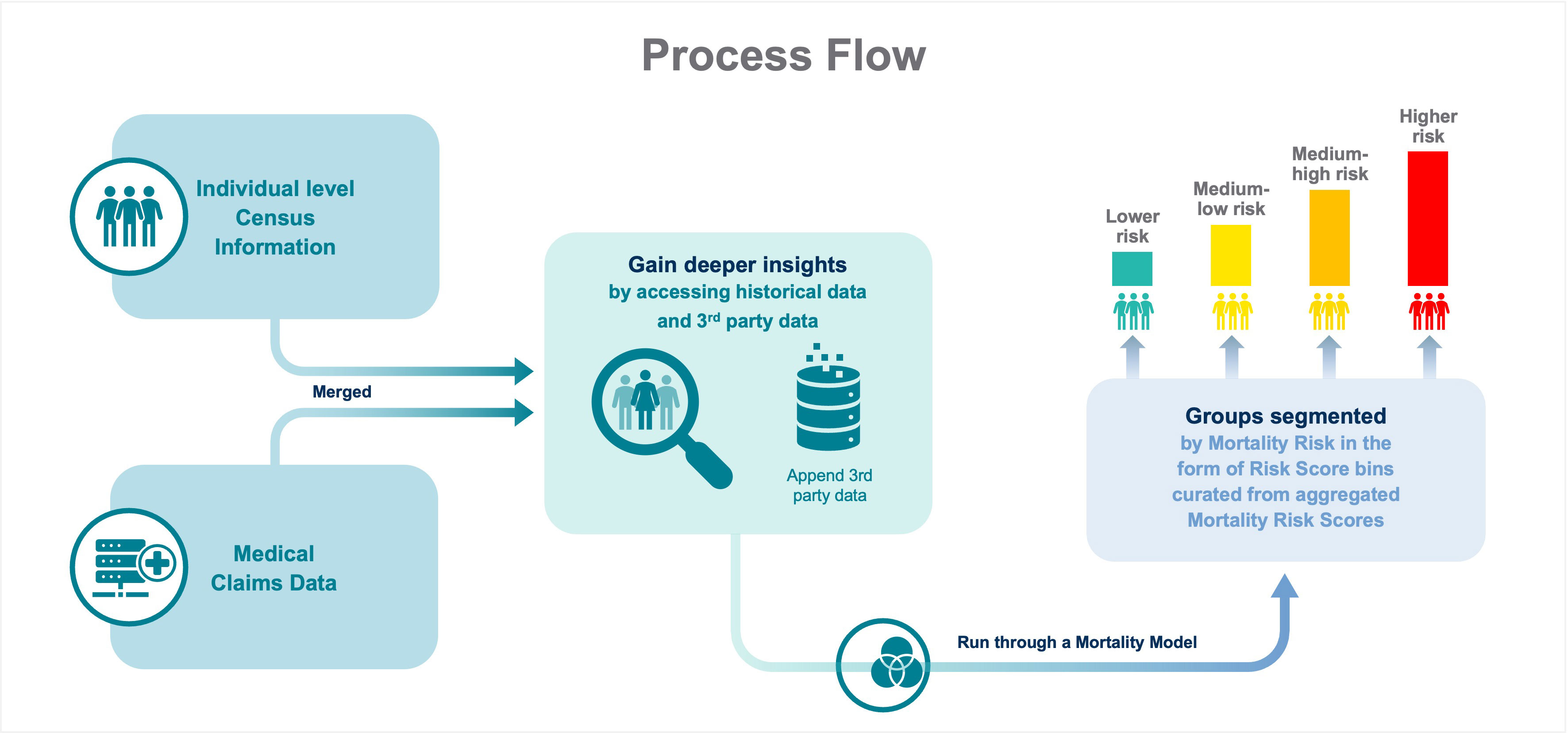
- Objective: The study was conducted to demonstrate the mortality-risk segmentation performance of the Munich Re Life US (Munich Re) medical billing mortality model with Group Life data. This model was built to predict mortality risk for individuals using medical billing claims information.
- Appending third-party data: The employer census was tokenized for privacy and joined to medical claims information.
- Mortality risk scoring: The medical claims information was run through the Munich Re medical billing mortality model, which produced a mortality risk score.
- Data aggregation: The model scored individuals and the score was then aggregated on the employer level. The aggregated score for each employer was used to evaluate the risk segmentation observed. This is one of many ways to restrict access to protected health information (PHI) within the process.
Risk score validation
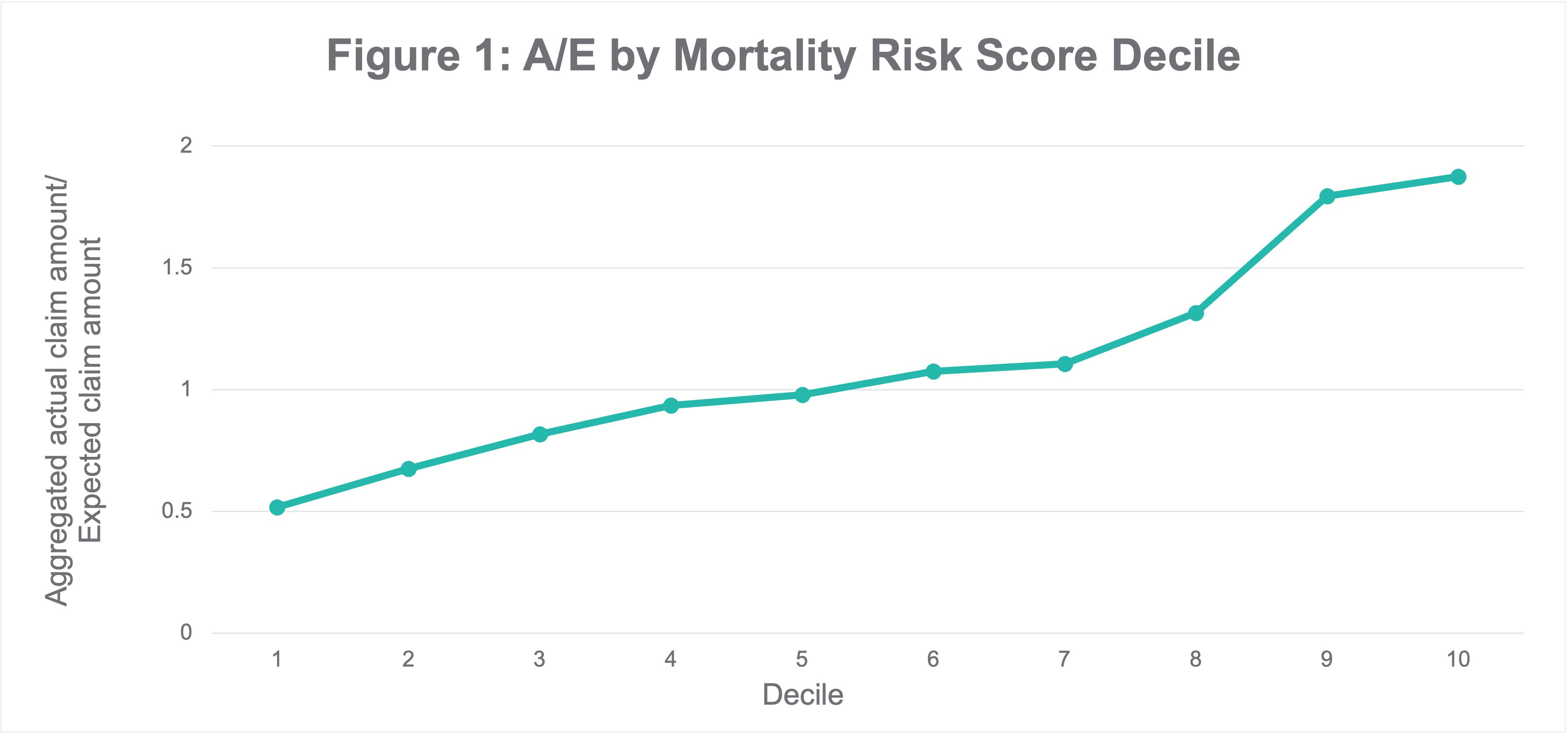
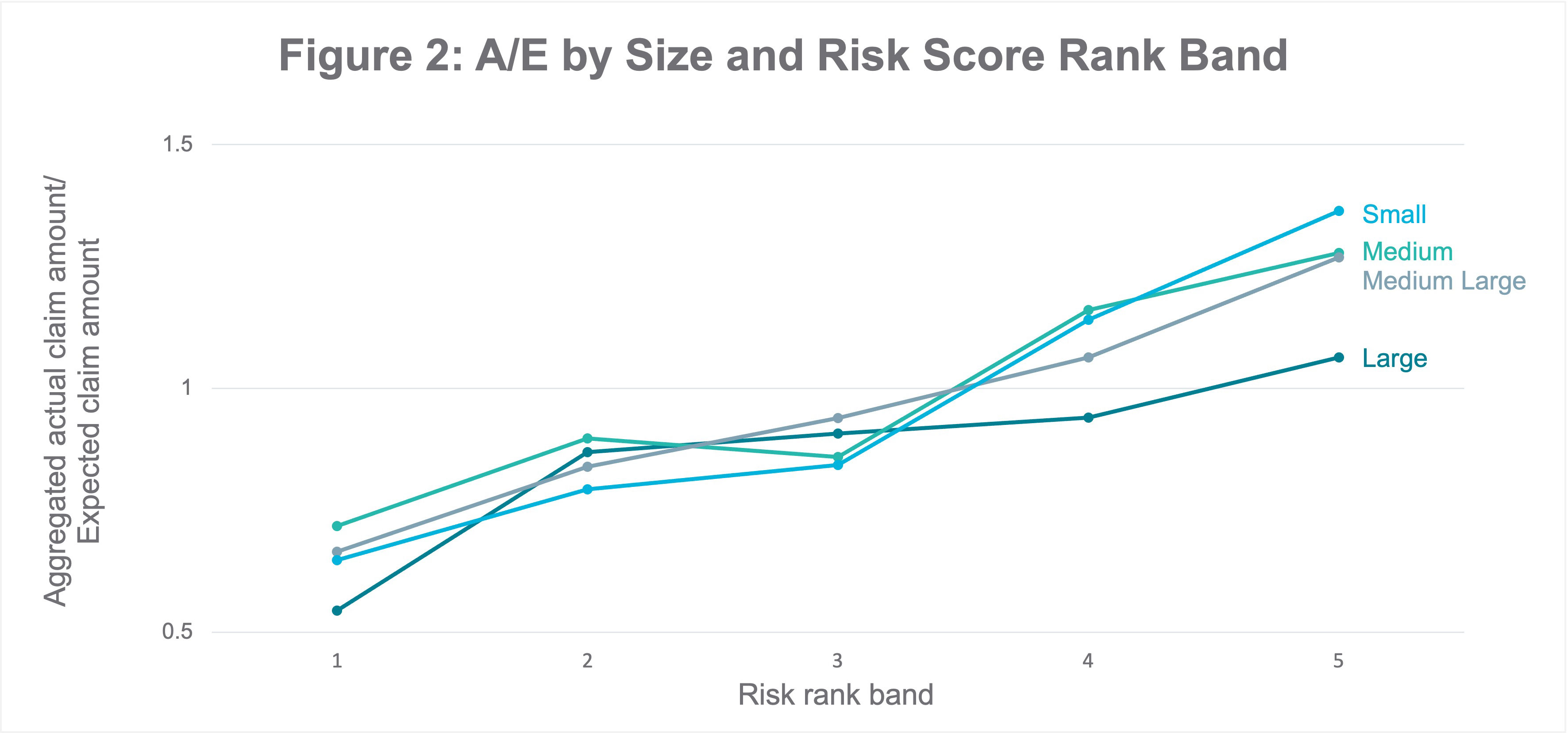
As a proxy for the Actual/Expected (A/E) ratio, we used a ratio of Paid Claim Amount/Expected Claim Amount, where the Expected Claim Amount is an estimate of the projected claim amount per employer and the Paid Claim Amount is the actual amount paid, to evaluate the mortality risk segmentation results from the scoring exercise described earlier. To analyze the trend, the employer-level risk score was binned into deciles, with each decile containing thousands of companies. We observed an upward slope in the aggregated A/E ratio across the risk bins, displaying segmentation between the bands to identify the employers with a good mortality risk profile (i.e., lower deciles), as shown in Figure 1 below.
A real-world use case
Jane is a Group Underwriter at an insurance company and is asked to provide a quote on a small to medium-sized employer’s application for a group life insurance policy. Since credible experience data is typically available only for larger cases, she finds that pricing based on the submission would rely heavily on the manual rate. Jane was provided basic census information, such as the name and date of birth of the employer’s current employees to determine the manual rate. To leverage this data even further, she:
- De-identifies the census information through tokenization
- Maps third-party medical data to it in a de-identified manner
- Runs the tokens through the mortality risk segmentation predictive model (referred to above)
- Gains insight into the distribution of employees across the different risk bands and finds that most of the employees fall within the lower mortality risk bins
Jane can then utilize this observation in many ways: to better profile the block of business with respect to mortality risk, adjust the manual rate and offer a competitive yet profitable rate for the case, set underwriting targets, and help price the program to apply additional discounts.
Incorporating the process into existing workflows
A predictive analytics process has limited effectiveness if it cannot be fully integrated into existing workflows. Incorporating third-party variables can allow a carrier to identify specific cohorts that are performing better or worse and to price the case more accurately. An automated pricing solution developed to capture the employer census, append third-party data, and perform calculations can return the appropriate load within minutes of the census being received. Integrating with external vendors can take many forms. Munich Re has successfully partnered with many carriers on efficient and effective ways to incorporate third-party data and model predictions into a pre-existing underwriting workbench.
Data hit rates and model performance should be monitored over time to ensure that current behavior meets the expectations set during any training or proof of concept stages. Periodic re-evaluation is also needed if consumer behavior or market conditions change to help ensure consistent, high performance from the data and models employed.
It is important to note that medical claims information, by nature, is less likely to be biased towards any groups of individuals when compared to socio-economic factors such as income and education. Incorporating findings from medical claims data in the underwriting and/or pricing process could thus help avoid bias in the workflow along with contributing to a more comprehensive risk assessment.
Conclusion
Making risk decisions with limited data can drive carriers to underprice business and ultimately sacrifice profits. This case study demonstrates that taking a data-driven predictive analytics approach can be a reliable and efficient approach to underwriting and pricing group risk.
Contact the Author

Newsletter
properties.trackTitle
properties.trackSubtitle