Advances in HIV Treatment

Technological advances in pharmacology, genetic engineering, genomics, and artificial intelligence are increasing the speed at which medical breakthroughs occur. These advances are creating fundamental changes to our understanding of health and medical treatment and could produce a lasting positive mortality and morbidity impact.
In this article series, the Munich Re medical team examines recent innovations in the field of medicine that are of particular interest to life and disability insurance carriers. Today we focus on new therapies for the treatment of HIV.
HIV: Still searching for a cure
Over 38 million people globally are estimated to be living with HIV, and another estimated 40 million people have died from the virus since its emergence in 1981.1 While new reports have declared that HIV is “cured”, this statement is only partially true. A stem cell transplant procedure, which interrupts the lifecycle of HIV cell replication in the body, has been successful in three patients to date with two others awaiting confirmation of cure.2 However, the procedure is not feasible for large populations due to its complexity, risk, and high cost of approximately $800,000 in the United States.
Antiretroviral therapy (ART), first introduced more than 30 years ago, remains today’s standard HIV treatment.3 This treatment uses a combination of drugs to suppress HIV replication by inhibiting various stages of the viral life cycle. A combination of HIV drugs is necessary because HIV can quickly adapt and become drug resistant. While we have seen great success with ART improving morbidity and mortality, it has not yet been able to cure the infection.
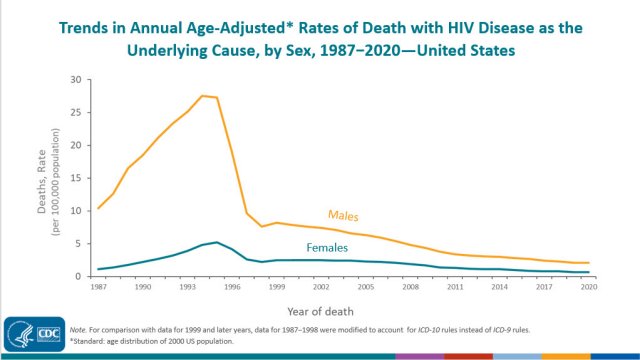
Even with declining death rates in response to antiretroviral therapies,4 the search for a cure is elusive due to the pernicious way that HIV integrates into cellular DNA. There is still no cure that can be broadly applied. Problems include integration of the viral DNA and reservoirs of infection unreached by current treatment. Specifically, some cells infected with the HIV virus lie dormant for quite some time or are not easily reached by various medications, e.g. in the central nervous system. As a result, the current regimens cannot fully eradicate the body of the virus.
Because of these difficulties, an important area of focus remains on prevention and early diagnosis and treatment, particularly for at-risk populations. Using condoms and safer sex practices greatly reduces the risk for getting HIV from an infected partner, and treatment as prevention of spread has made a huge impact on transmission of HIV. In addition, pre-exposure prophylaxis (PrEP) medications have been shown to reduce the chance of getting HIV from sex by 99% when taken as prescribed.5
Advances in HIV treatment
Preventative measures alone will never be enough to stop HIV infection. Fortunately, intense research focused on better understanding HIV, and advances in other areas of medicine, have produced several potential new treatment avenues. Solutions include methods that boost the immune system and T-cell turnover, utilize genetic approaches to either disable co-receptors required for viral attachment or eradicate the viral genome from cells, intensify ART, or prevent replication of latent proto-viruses.
One potential solution is the use of CRISPR gene editing to excise provirus DNA from the latent cells harboring it. This option is only theoretical at this time, as gene editing in humans is accompanied by a host of ethical, legal, and moral considerations, and would be a very expensive approach as well.
The development of an HIV vaccine would likely be the best option for wide deployment, as vaccines can be used in both preventative and therapeutic applications. There is a great deal of renewed interest in an HIV vaccine based on the lessons learned from Covid mRNA vaccine work. A study testing three experimental mRNA HIV vaccines is currently underway with the aim of understanding the vaccines’ safety and ability to stimulate immune responses against HIV. If the results are favorable, wider trials are expected.6
Underwriting and HIV
Understanding the impact of current therapies and what makes for the best risks allows for underwriting of many people with HIV. Morbidity continues to be driven by chronic inflammation resulting in accelerated atherosclerosis and increased risk for some cancers, along with psychiatric and neurodegenerative disease. A significant improvement in overall morbidity is achieved by individuals who are faithfully compliant with their treatment plans and exhibit favorable T-cell counts and HIV viral load levels.
2. https://www.forbes.com/sites/roberthart/2023/03/16/new-york-woman-cured-of-hiv-with-new-treatment/?sh=cf004a15486f; https://www.nih.gov/news-events/nih-research-matters/mixed-race-woman-potentially-cured-hiv-using-stem-cell-transplant#:~:text=Stem%20cell%20transplant%20remains%20a,expand%20access%20to%20this%20treatment
4. https://www.efpia.eu/publications/data-center/value-to-patients/hiv-death-rates/; https://www.cdc.gov/hiv/pdf/library/slidesets/cdc-hiv-surveillance-mortality-2020.pdf
5. https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html
6. https://covid19.nih.gov/news-and-stories/mrna-vaccine-technology-promising-idea-fighting-hiv
Contact the Author

Related Content
Newsletter
properties.trackTitle
properties.trackSubtitle



.jpg/_jcr_content/renditions/cropped.16_to_9.jpg./cropped.16_to_9.jpg)